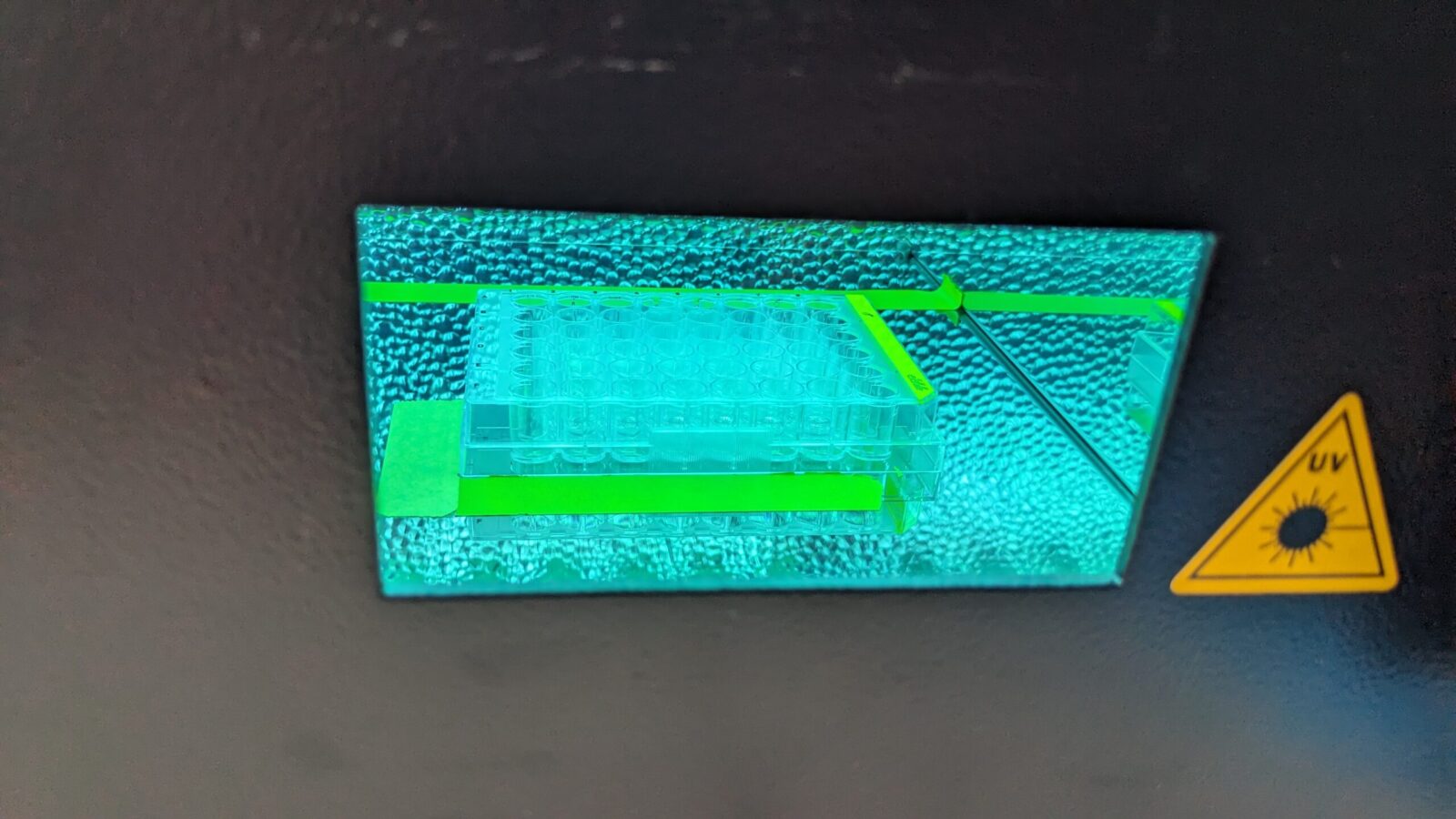
Dr. Eva Jablonská (University of Chemistry and Technology in Prague, Czech Republic) had a great opportunity to spend more than two months (15.1.-22.3.2024) at the Dermatotoxicology Study Centre, German Federal Institute for Risk Assessment (BfR) in Berlin. During the STSM granted by CA IMPROVE, she tested natural extracts from marine algae for photoprotective properties. Specifically, she irradiated human dermal fibroblasts with UV light and tested whether these extracts could prevent cellular damage.
Overall, the atmosphere at BfR was very welcoming and supportive. Additionally, the discussion about methods of genotoxicity testing were very fruitful.
Moreover, the grantee was fortunate to attend a three-day symposium on genotoxicity held by BfR, where quantitative approaches towards genotoxicity assessment were discussed.